What is dyslipidemia?
Dyslipidemia is an imbalance or dysfunction in the lipid profile. Commonly called “high cholesterol,” dyslipidemia has been associated with increased risks for heart disease and stroke. These are two of the leading causes of death, making dyslipidemia a major area of concern for cardiovascular well-being.
Is dyslipidemia different from hyperlipidemia?
While these terms are often used interchangeably, they are indeed different. In the past, healthcare practitioners focused more on the risks associated with elevated total cholesterol and elevated LDLs (low-density lipoprotein). For this reason, hyperlipidemia was a more common diagnosis and is still often used in clinical settings.
However, the healthcare community as a whole is shifting to the term dyslipidemia. Because a low HDL (high-density lipoproteins, which are considered “good cholesterol”) is also a risk factor for heart disease, the term hyperlipidemia does not properly describe the complete problem. Seeing the whole of a lipid profile provides a more comprehensive view of a patient’s cardiovascular health. Most recently, the role of elevated triglyceride is also apparent with respect to risk for vascular disease.
How do you diagnose hyperlipidemia?
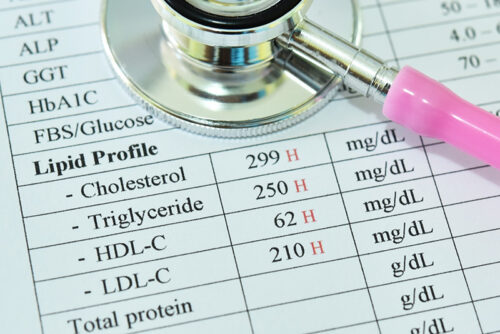
A serum lipid profile is a routine blood test. To be most accurate, patients should fast for up to 12 hours before the blood sample is drawn. However, a non-fasting lipid panel is better than no lipid panel, so beginning with non-fasting in the low-risk patient is fine. The lipid profile will measure four fats:
- Total cholesterol (Normal range <200 mg/dL)
- LDL cholesterol (Normal range <100 mg/dL)
- HDL cholesterol (Normal range > 40 mg/dL)
- Triglycerides (Normal range <150 mg/dL)
Of note: Some individuals have genetic dyslipidemia, causing abnormal levels of clinical concern. Clinicians should refer these patients to a specialist, such as an endocrinologist, for treatment and monitoring.
How widespread is hyperlipidemia?
In the U.S., over 90 million adults 20 or older have total cholesterol levels greater than 200 mg/dL, which is the “normal” threshold for healthy adults. Partly due to our diets and consumption of processed foods, it is common for American adults to have lipid levels outside of their optimal ranges.
However, because high cholesterol does not have symptoms, many patients do not know until they have a lipid panel done that they have dyslipidemia.
What are other risk factors associated with cardiovascular disease?
While certain lipid levels may require intervention immediately, other levels are borderline. In these cases, an individual’s goal lipid levels depend greatly on their other risk factors. When a patient has additional risk factors for cardiovascular disease, their lipid profile needs to be closer to optimal ranges. Some important risk factors include:
- Family history (heart disease, heart attacks, or stroke)
- Obesity
- Diabetes
- History of smoking/tobacco use
- Hypertension
- Stress
- Lack of exercise
- Poor diet
When does dyslipidemia require pharmacologic intervention?
There are certain goal levels for the lipid panel that medications can help achieve. There are also specific levels, mostly with LDLs, that should be treated immediately due to their cardiovascular risk. An LDL over 190 mg/dL needs to be treated immediately. Lower LDL levels may also require treatment, depending upon other patient factors, and very high risk patients may require treatment to an LDL < 70 mg/dL. The ACC/AHA has published an excellent set of algorithms to guide decision making.
What medications treat dyslipidemia?
Hmg-CoA reductase inhibitors, aka “statins” are the most common medications used in the treatment of dyslipidemia. Statins also provide other benefits, like stabilizing vascular cells and suppressing inflammation. Common statins include Lipitor, Crestor, and Zocor. Patients at very high risk for an atherosclerotic vascular event may need additional pharmacotherapy, and there are several other classes of medication that may be prescribed with a statin.
The American College of Cardiology and American Heart Association has guidelines for dyslipidemia treatment that uses statins as the first line of defense and can include other medications that may help raise HDLs or lower triglycerides, for example. Experts consider the polypharmacy approach as the best practice to achieve a lipid panel within normal ranges.
What lifestyle changes can help manage dyslipidemia?
When a patient has dyslipidemia, consider their diet and exercise. These are two highly important areas for managing dyslipidemia and cardiovascular health more generally. It would also be helpful for patients to quit smoking, try to lose weight, and make sure to get enough sleep, in order to best care for their cardiovascular health.
How does diet affect dyslipidemia?
Diet is an important factor in managing lipid levels. High-cholesterol foods like red meat, full-fat dairy, and fried foods should be consumed in moderation. Processed foods, like packaged meats and junk foods, should be avoided when possible. Food does not have to be high in cholesterol specifically to be problematic for patients with dyslipidemia. Foods with high saturated fat content and trans-fatty acids also affect lipid levels, as they affect the body’s production of these lipids.
Foods that have simple carbohydrates, like refined sugar and corn syrup, cause the body to produce more triglycerides, and foods with saturated fats cause the body to produce more LDLs. Therefore, an unhealthy diet can often be a cause of dyslipidemia.
What foods are good for patients with dyslipidemia?
Patients with dyslipidemia should follow heart-healthy eating tips to manage their lipid levels. Seafood and lean poultry are good options for protein-rich foods. Fish oil supplements are also helpful for raising HDLs if a patient does not eat seafood.
Vegetables, whole grains, beans, nuts, and seeds are other healthy food choices that can help manage dyslipidemia naturally.
Why is exercise important for treating dyslipidemia?
Aerobic exercise is an essential part of managing dyslipidemia. Exercise helps reduce cholesterol by raising HDLs and eliminating LDLs from the body.
The American Heart Association recommends 150 minutes of aerobic exercise of at least moderate intensity per week. Depending on a patient’s physical abilities, recommended exercises can include brisk walking, swimming, cycling, or yoga, among other things.
How do you monitor dyslipidemia treatment plans?
It is important to monitor a patient’s care to make sure you are moving in the right direction. If a patient is taking their medication and making efforts to change their lifestyle, this is a good sign for their cardiovascular health.
However, anytime a medication change occurs, it is important to recheck the lipid panel to ensure the treatment is working. Once a treatment plan stabilizes, reassess the patient’s lipid profile annually or every six months to make sure their numbers are moving in the correct direction.
Dyslipidemia is a complex but manageable condition. Working with patients to make comprehensive lifestyle changes is the best way to reduce their risk of cardiovascular disease and keep dyslipidemia at bay.
Earn CE hours by listening to the Diagnosing and Managing Dyslipidemia podcast (free with Passport Membership)!